Menopause and sleep are inextricably linked, with hormonal changes during this life stage significantly impacting the quality and duration of rest. This article delves into the complexities of this relationship, exploring the causes, symptoms, and treatment options for sleep disturbances in menopause.
Menopause and Sleep
Menopause is a natural biological process that marks the end of a woman’s reproductive years. It typically occurs between the ages of 45 and 55, but can vary from woman to woman. Menopause is characterized by a decline in the production of the hormones estrogen and progesterone, which can lead to a range of physical and emotional changes, including sleep disturbances.
Stages of Menopause
Menopause is typically divided into three stages:
- Perimenopause:This stage begins several years before menopause and is characterized by fluctuating hormone levels, which can lead to irregular periods, hot flashes, and other symptoms.
- Menopause:This stage is defined as the point at which a woman has not had a period for 12 consecutive months. It typically occurs between the ages of 45 and 55.
- Postmenopause:This stage begins after menopause and lasts for the rest of a woman’s life. During this stage, hormone levels are stable and most symptoms of menopause subside.
Hormonal Changes and Sleep
The hormonal changes that occur during menopause can have a significant impact on sleep. Estrogen and progesterone are both known to play a role in regulating sleep. Declining levels of these hormones can lead to:
- Hot flashes:Hot flashes are a common symptom of menopause that can disrupt sleep. They are caused by a sudden drop in estrogen levels, which triggers the body’s temperature regulation system to overreact.
- Night sweats:Night sweats are another common symptom of menopause that can disrupt sleep. They are caused by the same hormonal changes that cause hot flashes.
- Changes in sleep architecture:Menopause can also lead to changes in sleep architecture, which is the pattern of sleep stages that occur throughout the night. These changes can include a decrease in deep sleep and an increase in light sleep.
Symptoms of Sleep Disturbances in Menopause
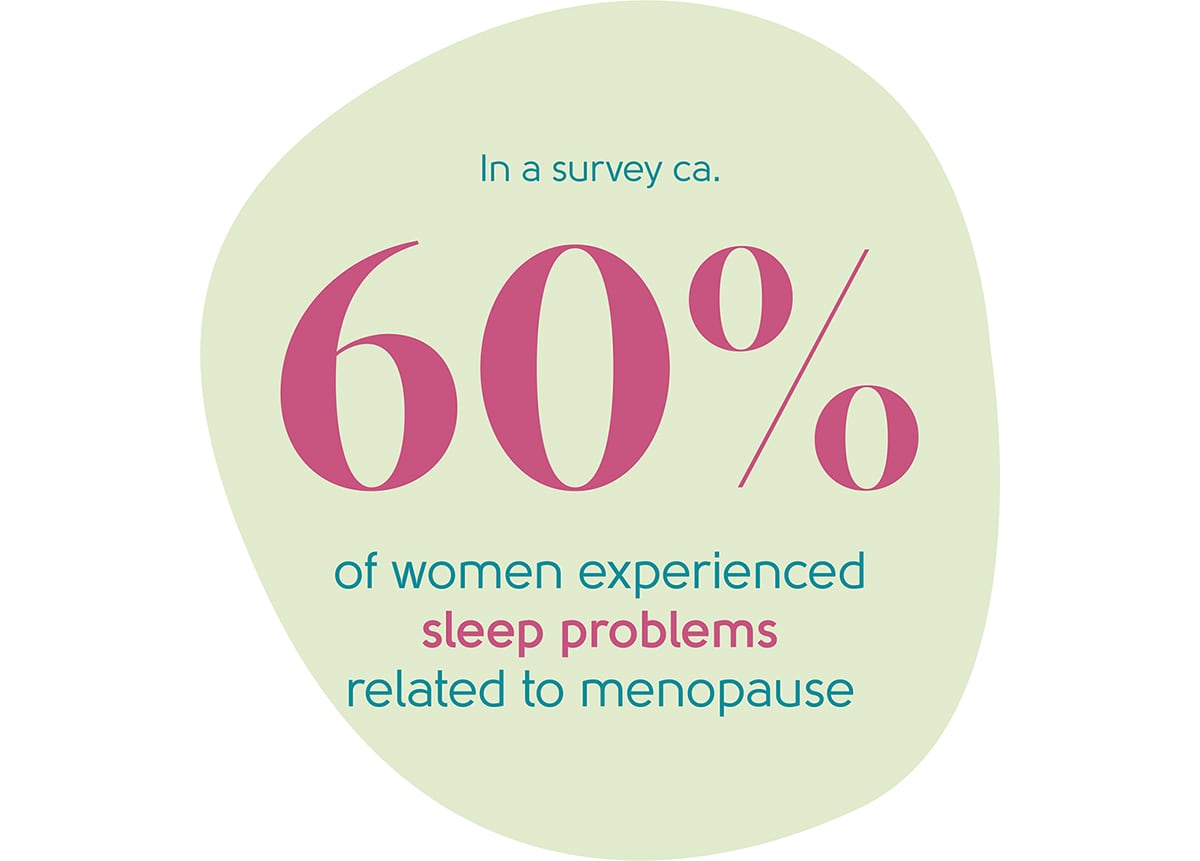
Sleep disturbances are common during menopause, affecting up to 60% of women. These disturbances can range from mild to severe and can significantly impact daily life.
Common Sleep Problems
- Insomnia:Difficulty falling or staying asleep, waking up frequently during the night, or waking up too early in the morning.
- Hot flashes:Sudden feelings of intense heat that can cause sweating, heart palpitations, and difficulty sleeping.
- Night sweats:Excessive sweating during sleep, which can lead to frequent awakenings and disrupted sleep.
- Sleep apnea:A condition where breathing repeatedly stops and starts during sleep, leading to poor sleep quality and daytime sleepiness.
- Restless legs syndrome (RLS):An uncomfortable sensation in the legs that worsens at night, making it difficult to fall or stay asleep.
The severity of these sleep problems can vary from woman to woman. Some women may experience only mild symptoms that do not significantly interfere with their daily lives, while others may experience severe symptoms that disrupt their sleep and overall well-being.
For example, insomnia can lead to fatigue, difficulty concentrating, and irritability. Hot flashes and night sweats can cause discomfort and interrupt sleep, leading to daytime sleepiness and impaired performance. Sleep apnea can increase the risk of cardiovascular disease and other health problems.
Causes of Sleep Disturbances in Menopause
Sleep disturbances are a common symptom of menopause, affecting up to 60% of women. These disturbances can range from difficulty falling asleep to waking up frequently during the night. There are a number of factors that can contribute to sleep problems in menopause, including physiological and psychological changes.
Physiological Factors
One of the most significant physiological changes that occurs during menopause is a decline in estrogen levels. Estrogen is a hormone that helps to regulate sleep. When estrogen levels decline, it can lead to changes in the body’s sleep-wake cycle, making it more difficult to fall asleep and stay asleep.
Another physiological factor that can contribute to sleep disturbances in menopause is vasomotor symptoms, such as hot flashes and night sweats. These symptoms can disrupt sleep by causing women to wake up feeling hot and uncomfortable.
Psychological Factors
In addition to physiological changes, psychological factors can also contribute to sleep problems in menopause. These factors include stress, anxiety, and depression.
Stress is a common trigger for sleep problems. When women are stressed, they may have difficulty falling asleep or staying asleep. Anxiety is another common trigger for sleep problems. Women who are anxious may worry about their health, their finances, or their relationships, which can make it difficult to fall asleep.
Depression is a serious mental illness that can also lead to sleep problems. Women who are depressed may have difficulty falling asleep, staying asleep, or waking up feeling refreshed.
Treatment Options for Sleep Disturbances in Menopause
Sleep disturbances are a common symptom of menopause, affecting up to 60% of women. There are a variety of treatment options available to help improve sleep quality during this time.
Treatment options for sleep disturbances in menopause can be divided into three main categories: lifestyle changes, hormonal therapy, and medications.
Lifestyle Changes
Lifestyle changes are often the first line of treatment for sleep disturbances in menopause. These changes can help to improve sleep hygiene and create a more conducive environment for sleep.
- Establish a regular sleep schedule and stick to it as much as possible, even on weekends.
- Create a relaxing bedtime routine that helps you to wind down before bed.
- Avoid caffeine and alcohol before bed.
- Make sure your bedroom is dark, quiet, and cool.
- Get regular exercise, but avoid exercising too close to bedtime.
- Avoid smoking.
Hormonal Therapy
Hormonal therapy can be an effective treatment option for sleep disturbances in menopause. Hormone replacement therapy (HRT) can help to reduce hot flashes and night sweats, which can interfere with sleep.
- Estrogen therapy can be taken orally, transdermally (through the skin), or vaginally.
- Progestin is often added to estrogen therapy to reduce the risk of endometrial cancer.
Medications
Medications can be used to treat sleep disturbances in menopause when lifestyle changes and hormonal therapy are not effective.
- Over-the-counter sleep aids, such as diphenhydramine (Benadryl) and doxylamine (Unisom), can be effective for short-term use.
- Prescription sleep aids, such as zolpidem (Ambien) and eszopiclone (Lunesta), can be effective for longer-term use.
- Antidepressants, such as trazodone (Desyrel) and mirtazapine (Remeron), can also be effective for treating sleep disturbances in menopause.
The best treatment option for sleep disturbances in menopause will vary depending on the individual woman’s symptoms and preferences. It is important to discuss the benefits and risks of each treatment option with a doctor before making a decision.
Lifestyle Modifications for Improving Sleep in Menopause
Menopause can bring about a myriad of changes in a woman’s body, including sleep disturbances. However, there are several evidence-based lifestyle modifications that can significantly improve sleep quality during this transition.
Sleep Hygiene
Establishing good sleep hygiene practices is crucial for restful sleep. This includes:
- Going to bed and waking up at the same time each day, even on weekends.
- Creating a relaxing bedtime routine, such as taking a warm bath, reading, or listening to calming music.
- Avoiding caffeine and alcohol before bed.
- Ensuring the bedroom is dark, quiet, and cool.
Exercise
Regular exercise can promote better sleep. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Avoid exercising too close to bedtime, as this can interfere with sleep.
Diet
Certain dietary changes can improve sleep quality. For example:
- Eating a balanced diet that includes plenty of fruits, vegetables, and whole grains.
- Limiting processed foods, sugary drinks, and unhealthy fats.
- Avoiding large meals before bed.
Stress Management
Stress can significantly disrupt sleep. To manage stress, consider:
- Practicing relaxation techniques such as yoga, meditation, or deep breathing.
- Getting enough sleep, as sleep deprivation can worsen stress.
- Seeking professional help if stress is severe or persistent.
Role of Healthcare Professionals in Managing Sleep Disturbances in Menopause
Healthcare professionals play a pivotal role in diagnosing and managing sleep disturbances in menopause. They possess the expertise to assess the underlying causes, provide appropriate treatment options, and offer guidance and support to patients.
Patient Education and Support
Healthcare professionals have a responsibility to educate patients about the physiological changes associated with menopause and their impact on sleep. They can provide information on common sleep disturbances, their symptoms, and potential triggers. Additionally, they can offer reassurance and support, helping patients understand that sleep disturbances are a normal part of the menopausal transition.
Collaboration for Improved Sleep
Healthcare professionals can collaborate with patients to develop individualized treatment plans that address their specific sleep concerns. This may involve lifestyle modifications, such as establishing regular sleep-wake cycles, optimizing the sleep environment, and engaging in relaxation techniques. In some cases, they may prescribe medications or recommend alternative therapies to alleviate sleep disturbances.
Case Studies of Successful Interventions for Sleep Disturbances in Menopause

Numerous women have successfully managed their sleep disturbances during menopause through various interventions. These case studies highlight the importance of individualized treatment plans and the effectiveness of tailored approaches.
Hormone Replacement Therapy (HRT)
- Case Study:A 52-year-old woman experienced severe hot flashes and night sweats, leading to fragmented sleep and daytime fatigue. HRT with estrogen and progesterone alleviated her symptoms, significantly improving her sleep quality and duration.
- Case Study:A 55-year-old woman reported difficulty falling and staying asleep, accompanied by anxiety and mood swings. HRT with estrogen-only therapy improved her sleep onset latency and sleep maintenance, reducing her sleep disturbances.
Cognitive Behavioral Therapy for Insomnia (CBT-I), Menopause and sleep
- Case Study:A 53-year-old woman struggled with insomnia, characterized by excessive worry and negative thoughts at bedtime. CBT-I helped her identify and challenge her sleep-related beliefs, develop relaxation techniques, and establish a regular sleep-wake cycle, resulting in improved sleep.
- Case Study:A 56-year-old woman experienced sleep disturbances due to menopause and work-related stress. CBT-I provided her with coping mechanisms for stress management, cognitive restructuring, and behavioral interventions, effectively reducing her sleep problems.
Lifestyle Modifications
- Case Study:A 54-year-old woman with mild sleep disturbances implemented lifestyle changes, including regular exercise, a healthy diet, and a relaxing bedtime routine. These modifications reduced her stress levels, improved her overall well-being, and consequently enhanced her sleep quality.
- Case Study:A 57-year-old woman found relief from sleep disturbances by creating a conducive sleep environment, maintaining a cool room temperature, and using blackout curtains to minimize light exposure. These adjustments optimized her sleep environment, leading to better sleep.
Future Research Directions in Menopause and Sleep
Research on menopause and sleep continues to expand our understanding of the complex relationship between these two factors. However, several gaps in knowledge still exist, providing ample opportunities for future research endeavors.
Emerging Technologies and Innovative Approaches
The advent of new technologies and innovative approaches holds promise for improving sleep in menopausal women. Future research should explore the potential of:
- Wearable sleep trackers:These devices can provide objective data on sleep patterns, helping researchers and clinicians identify and address sleep disturbances.
- Mobile health (mHealth) interventions:Smartphone-based apps and other mHealth tools can deliver personalized sleep interventions, such as cognitive behavioral therapy for insomnia (CBT-I) and relaxation techniques.
- Non-invasive brain stimulation:Techniques like transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) may offer novel approaches to improve sleep quality.
Closing Notes: Menopause And Sleep
Understanding the interplay between menopause and sleep is crucial for women navigating this transition. By addressing sleep disturbances effectively, women can improve their overall well-being and quality of life during menopause and beyond.
FAQ Section
Can hormonal therapy help improve sleep during menopause?
Hormonal therapy, such as estrogen or progesterone, can alleviate vasomotor symptoms and mood changes that contribute to sleep disturbances.
What lifestyle changes can improve sleep in menopause?
Establishing a regular sleep schedule, engaging in regular exercise, and managing stress through techniques like yoga or meditation can promote better sleep.
How can I cope with night sweats and hot flashes that disrupt sleep?
Wearing loose, breathable clothing, using cooling sheets or a fan, and avoiding caffeine and alcohol before bed can help mitigate these symptoms.